This time last year I wrote about five policy priorities to improve maternal health in Iowa. I’m updating the piece for the 2024 session with a focus on three core priorities for the 2024 session.
Similar to last year, while access to abortion care and contraceptives are critical to maternal and infant health, I do not include them in these maternal health policy priorities. The focus of my articles are on aspects of maternal health specific to prenatal, birth, and postpartum care that are less widely known by Iowans and much less covered by media outlets.
For the 2024 legislative session, I am focusing on three issues that I highlighted in 2023 that I think have promise in being implemented in some way or another. All three of these issues are important to improving maternal health in Iowa by expanding access to midwives and expanding prenatal care options. I wrote at length in 2021 about how midwives save lives and it seems like every week a different study or article speaks to how critical the midwifery model of care is to improving outcomes. If you’re interested in diving deeper, one of my favorite resources released in 2023 is this Issue Brief on Maternity Medicaid Strategies from the Maternal Health Hub.
I think it is also important to acknowledge that infant mortality increased in 2022 for the first time in 20 years. As reported by The Associated Press, “More than 30 states saw at least slight rises in infant mortality rates in 2022, but four states had statistically significant increases — Georgia, Iowa, Missouri and Texas.”
Two of the main reasons attributed to the increase in infant mortality are due to poverty and inadequate prenatal care. With almost one-third of Iowa being classified as a maternal health desert, the policy solutions I am proposing have the potential to improve access to prenatal care in rural areas by expanding low-cost and high quality prenatal care options that would improve outcomes for both moms and babies.
Expand access to freestanding birth centers and exempt birth centers from Certificate of Need
As I wrote last year, Certified of Need (CON) laws lead to increased healthcare costs, make it harder for individuals like midwives to establish freestanding birth centers, and create fewer options for Iowans seeking prenatal, birth, and postpartum care. If you didn’t read my previous article, here is a quick recap of why this matters:
- According to the American Association of Birth Centers, certificate of need laws are associated with fewer birth centers in a state. Research has shown birth centers improve outcomes, narrow racial disparities, enhance patient satisfaction, and reduce costs to state Medicaid programs and other payers.
- Iowa is in the minority of states that require a certificate of need for birth centers (less than 15 states). Among nearby states, Minnesota, South Dakota, Nebraska, Kansas, Missouri, and Wisconsin do not require a certificate of need for birth centers. (Note, I’m really tired of Iowa media outlets incorrectly reporting on birth center specific CON laws in other states. They often don’t do the extra work of finding that while more states have CON laws, many exempt birth centers!)
- This 2019 report confirmed that birth centers deliver improved health outcomes at a lower cost, averaging 21 percent lower cost of birth and 15 percent lower cost for care for women and infants for the first year after birth.
- The Institute for Medicaid Innovation’s 2020 report on Improving Maternal Health Access, Coverage, and Outcomes in Medicaid indicated that midwife-led care—including in freestanding birth centers—results in improved care, better outcomes, and costs less.
A few things have changed since last year including the only freestanding birth center in Iowa closed making Iowa one of only a handful of states without any freestanding birth centers. Also Pacific Legal Foundation took on a pro bono legal case on behalf of two Certified Nurse Midwives (CNMs), Caitlin Hainley and Emily Zambrano-Andrews who want to open a freestanding birth center. Hainley and Zambrano-Andrews are CNMs providing primary care, gynecological, pregnancy, and lactation services in their Des Moines based clinic. They provide home birth services, but are unable to open a freestanding birth center without going through the expensive Certified of Need process with no guarantee of success. I am hard pressed to think of an example of any other small business having to jump through similar hoops to start a business, let alone a business that would meet a pressing need.
During the 2023 session, SF 506 passed the Senate (29-21) with all Democrats voting against the bill. The bill is a broad reform of Certificate of Need that would increase the financial thresholds of health care facilities that would need to go through CON. The bill would also eliminate the Health Facilities Council and instead have the CON application process administered by the Department of Inspections, Appeals, and Licensing (this is my reading of the bill but reference to “department” could refer to another agency like HHS). Additionally the bill would remove birth centers and community mental health centers from the process. The bill could now be considered by the House Health and Human Services Committee.
It is unclear to me why Senate Democrats would oppose this bill and want to protect the Health Facilities Council. Eliminating or improving Certificate of Need should be a bipartisan issue, even if it is being led primarily by pro-business and anti-regulation organizations. I am not naive enough to assume most of those advocating for the elimination of CON care at all about improving health care outcomes. They are interested in making money for their mostly physician clients. That being said, maintaining CON only serves to protect hospitals as monopolies in a state with very little accountability for their outcomes.
As noted by this 2021 Forbes article, “Demonstrating the potential for bipartisan cooperation on this issue, the need to repeal or reform CON requirements was a rare instance of agreement between the Obama and Trump administrations.”
The same Forbes article mentions, “Controlling for other factors, researchers find that the average patient in a CON state has access to fewer hospitals, fewer hospice care facilities, fewer dialysis clinics and fewer ambulatory surgery centers (ASCs)”.
When it comes to access to healthcare, Iowa is already on the struggle bus. CON laws make it harder for midwives like Hainley and Zambrano-Andrews to open a birth center. As I have written before, there are other midwives in Iowa that have tried to open a birth center and were denied through the CON process.
While I support SF 506 for removing birth centers from CON, I do take pause at the amendments made related to birth centers at the request of hospital lobbyists. The amended bill requires the Department of Inspection, Appeals, and Licensing to create a provisional birth center licensure and proposed birth center licensure legislation the following year.
Any proposed birth center licensure should be developed with input from experts like those at the American Association of Birth Centers (AABC). While I see value in establishing standards for freestanding birth centers in Iowa, I am apprehensive about eliminating one barrier to create another, if not done properly. Just this past year, the ACLU sued the Alabama Department of Public Health due to its “defacto ban on birth centers” per their birth center licensure being unattainable. The case is ongoing, while Alabama’s first licensed birth center opened in December thanks to a preliminary injunction.
Some glimmers of hope from the federal level include a new model from the Centers for Medicare and Medicaid Services (CMS) released in December, which includes a focus on increasing access to midwives and birth centers. States wanting to receive funding from CMS related to the model will need to be willing to make way for freestanding birth centers. For Iowa this could mean not only exempting birth centers from CON, but also making sure Medicaid funding is accessible. As of today, the state is not in compliance with having a birth center fee schedule.
Several bipartisan federal pieces of legislation have been proposed in recent years that would uplift midwifery and birth centers. The Midwives for MOMS Act was introduced in June 2023 in the House by Iowa’s own Representative Ashley Hinson (R-IA) and Representative Bonnie Watson Coleman (D-NJ), and in the Senate by Senators Ben Ray Lujan (D-NM) and Lisa Murkowski (R-AK), which would provide funding for midwifery education.
The BABIES Act seeks to promote accessible and affordable use of freestanding birth centers by Medicaid Beneficiaries and was sponsored in the House by Assistant Speaker Katherine Clark (D-MA-5) and original co-sponsors Representative Jaime Herrera Beutler (R-WA-3), Representative Lucille Roybal-Allard (D-CA-40), and Representative Ashley Hinson (R-IA-1). As of October 12, 2022, there are 46 co-sponsors in the House. In the Senate, the BABIES Act is sponsored by Senator Ben Ray Luján (D-NM).
The Black Maternal Health Momnibus Act is a comprehensive compilation of 13 individual bills that would improve perinatal care and diversity in the perinatal workforce with a focus on maternal health disparities, including access to the midwifery model of care.
Whether it is through legislation, a lawsuit, or federal funding, I hope CON will soon be one less barrier to Iowans having access to freestanding birth centers.
Improvements to Medicaid Coverage
Talking about improvements to Medicaid coverage may seem like a longshot when it comes to politics in Iowa, yet when more than 40% of Iowa births are covered by Medicaid, you would be hard pressed to find a legislator of any political affiliation that doesn’t understand the importance Medicaid plays in maternal and infant health outcomes.
The big push in 2024 will be to implement 12 months of Medicaid coverage postpartum from the 60 days currently provided in Iowa. As of today, Iowa is one of only three – yes you read that correctly – only three states including Arkansas, Idaho, and Iowa have yet to adopt 12 months of postpartum Medicaid coverage. There is a broad coalition of organizations led by Iowa ACEs 360 collaborating to make the case for Iowa to adopt 12 months postpartum Medicaid coverage.
Some of the most dangerous pregnancy-related complications (i.e., eclampsia, blood clots, cardiomyopathy, strokes) may not surface until months after delivery. Without access to health coverage, these conditions can go undetected and untreated, sometimes turning deadly. Per the 2021 Iowa Maternal Mortality Review Committee Report, over half (54%) of Iowa’s pregnancy-associated deaths occurred within 43-days to 1 year after birth.
Suicide and overdose are the leading causes of death in the first year postpartum with the 3-6 month timeframe as the most critical for mental health issues developing and 6-9 months the timeframe when most pregnancy related suicides occur per the Maternal Mental Health Alliance. It is important to note that while suicide and overdose are the leading cause of death for the majority of new mothers, when you break this down by race it is only the leading cause for white women and hispanic women. The leading cause of death for Black women is cardiac and coronary conditions and the leading cause for Asian women is hemorrhage.
Maternal mortality and morbidity from untreated pregnancy related or associated conditions have an impact on Iowa’s economy. Maternal health issues may affect the ability to work and can create significant losses in the family’s economic productivity. A study by Commonwealth Fund found that over a five year period, maternal morbidity cost the United States $6.6 billion in lost productivity. The estimated total maternal morbidity costs for all U.S. births in 2019 is estimated to be $32.3 billion from conception through the child’s fifth birthday. This amounts to $8,624 in additional costs to society for each maternal–child pair.
In Missouri the 12 months postpartum Medicaid coverage bill that passed in 2023 was sponsored by Republican Senator Elaine Gannon with a message that the potential cost of the program was worth it if it meant saving lives. I agree, and while I don’t have data to support this given 12 months postpartum coverage is still new, my strong assumption is it not only saves lives, but it will also save states money in the long run with fewer downstream health consequences impacting an already strained healthcare system.
Something to be proud of is that Iowa currently provides Medicaid coverage for pregnant individuals that are at or below 380% of the Federal Poverty Level (FPL) through pregnancy and currently up to 60 days postpartum. A concern is that in order to pass a bill to extend coverage to 12 months postpartum, there will be a compromise to scale back the FPL to a lower number and cover fewer women. While 380% may seem high, research shows that 15.1% of pregnant and 18.3% of postpartum people with commercial insurance face medical debt, making them effectively underinsured.
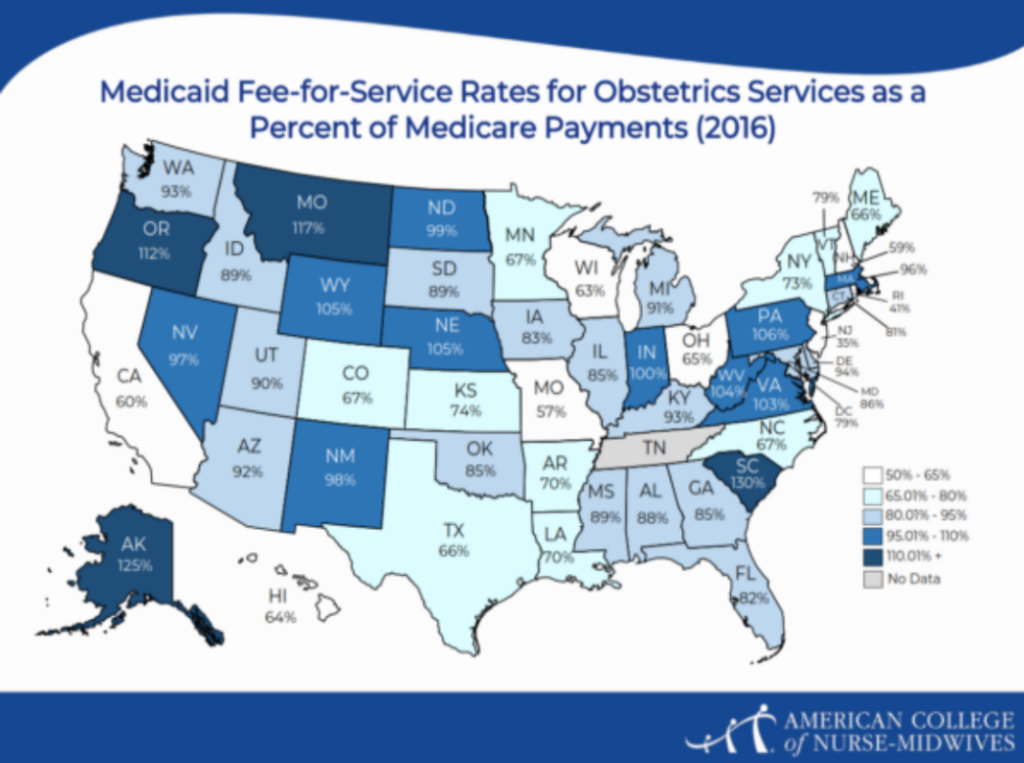
Something I shared last year is we also need to increase the reimbursement for Certified Nurse Midwives and OBGYN providers for the global obstetric fee-for-service reimbursed by Medicaid in Iowa, which covers all prenatal, birth, and postpartum care. The reimbursement is so nominal it is hardly worth the paperwork to become a Medicaid provider. This inordinately affects Certified Nurse Midwives who provide these services for those seeking out of hospital birth. There is currently only one out-of-hospital practice within 300 miles of Des Moines practice that accepts Medicaid.
I recently learned that doulas, part of the state’s pilot doula project, receive $1,000 per client. While I think doulas are deserving of that fee, this is compared to only $1,159.80 Certified Nurse Midwives are receiving for Medicaid homebirth clients – including the entire ten months of pregnancy, as well as the two months of postpartum care and any lactation care provided. This is less than $100/month for ensuring the health and safety of a mother and baby. It is no wonder almost no home birth CNM providers currently accept Medicaid. The state must update its provider fee schedule to ensure homebirth providers are receiving adequate reimbursement.
The last area related to Medicaid improvements is what should be an easy fix to end pay disparities for Certified Nurse Midwives who are reimbursed at only 85% of the rate the state reimburses physicians when providing the same services for gynecological and obstetrical care such as pap smears, contraceptive family planning, prenatal/postpartum care, and vaginal deliveries. It is no wonder hospitals across the state devalue midwives when they are reimbursed 15% less by the state for the same work of physicians. Physicians are already paid more for cesareans and other specialities they provide so it is not as if they are not getting paid equitably for their services.
While the gender makeup of most OBGYNs now skews to women, the inequity of paying the profession with men in it more than women nurse-midwives (I don’t know any male midwives in Iowa) for the same work is pretty obvious. While “Equal Pay Day” is recognized every March to recognize the gender wage gap of women working full-time earning an average of 83.7 percent as much as men, you don’t need a hypothetical “equal pay day” to demonstrate how the state of Iowa is discriminating against the female workforce of midwives.
When I have raised the issue of pay equity for CNMs, I’ve been told this is something that must be solved by the legislature. I would welcome a legislator to take up this issue (see sample legislation from Connecticut here). That being said, I cannot find in state law where it says CNMs must be paid 85% of physicians for the same work. What I find related to reimbursement is in Iowa HHS Administrative Code chapter 79 which refers to the Advanced Registered Nurse Practitioner (ARNP) fee schedule. If it is only in administrative code, I would assume this is something the Department of Health and Human Services could solve through rulemaking. Whether in law or administrative rules, there is also an opportunity for the Managed Care Organization (MCOs) to reimburse higher than the 85%. In some states MCOs reimburses for midwifery care at higher rates, with an MCO in Georgia reimbursing 108% of physician pay for midwives for “value-based care” (also known as better outcomes).
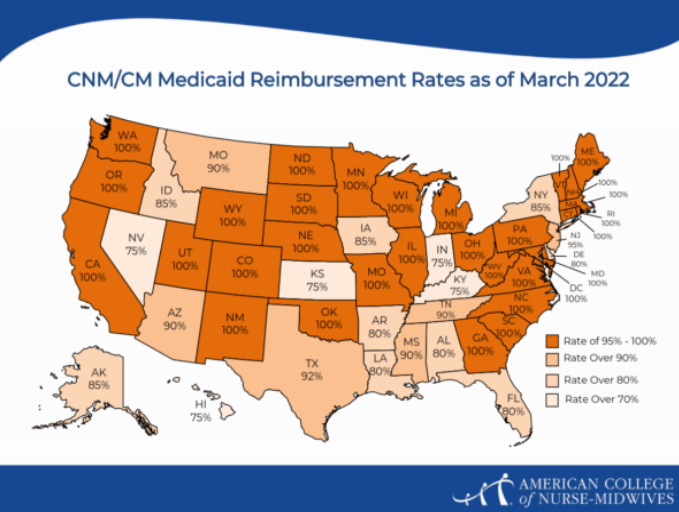
Iowans should not shy away from expecting better Medicaid coverage to improve care options and outcomes. Looking at other Republican controlled states who are leading the way, we can have 100% or more of the global obstetric Medicaid fee for service set by CMS, 100% CNM reimbursement, and 12 months postpartum coverage. If we are asking for 12 months postpartum coverage, to improve access to care we must also be asking for 100% CNM reimbursement, and a higher obstetric Medicaid reimbursement fee.
Fully Implement Certified Professional Midwives Licensure
Everyone was probably hoping they were done reading about Certified Professional Midwives from me once Governor Reynolds signed HF 265 into law on June 1, 2023. The bill had overwhelming bipartisan support passing the Senate 46-2 and the House 91-2. The bill provides licensure for Certified Professional Midwives (CPMs), increasing access to quality maternal health care providers. Licensure is necessary for CPMs to obtain the life saving medications within their training and scope of practice. You can read my comprehensive write-up “The time has come to finally license midwives in Iowa” on why CPM licensure was necessary.
Getting the bill passed came down to the wire with a compromise amendment made in the Senate led by Floor Manager Senator Scott Webster, to avoid the creation of a new board and to keep the licensing fee low. The compromise was to have the licensure administered by the Board of Nursing and to create a “Midwifery Advisory Council” that will “advise the board regarding licensure and continuing education requirements, standards of practice, professional ethics, disciplinary actions, and other issues relating to midwifery.”
The Governor recently appointed the inaugural MAC members and licensure is supposed to be available by July 1, 2024. The hiccup is the Boards and Review Committee’s Final Report issued in September 2023 recommends eliminating the MAC. According to the report, “The statute is highly prescriptive, and the Board of Nursing can administer licensure without the Council.” What the review committee misses is that CPMs are not nurses and those serving on the Board of Nursing, which has a significant workload as it is, will likely never have expertise in the practice of midwifery.
The legislature overwhelmingly passed the bill to create the MAC as an advisory group to the Board of Nursing, which is in alignment with the intent of the Board and Review Committee to save the state money and avoid a new entity administering the licensure. Having a different profession, in this case nurses, set CPM rules creates barriers for the CPM workforce and is contrary to the goals of the Boards and Commissions Review Committee goals and recommendations.
Hopefully the MAC will be retained, but if a bill is proposed in alignment with the Boards and Review Committee’s recommendations, legislators will need to hear from Iowans that the Midwifery Advisory Council should be maintained. We should not disrupt the implementation of a new law providing oversight to a critical maternal health workforce before it has even had a chance to begin issuing licenses.
There is a lot more that could be said about the historic passage of HF 265, who supported it or more specifically who didn’t support it going against evidence based research and public health recommendations. Given the significant support of HF 265 in the legislature, I remain hopeful that the MAC will be retained. That being said, I also recognize there will be a lot of competing priorities in the 2024 legislative session. Hopefully we can finally celebrate in July with the newly licensed midwives.
—
I hope after reading these policy priorities you will take a few minutes to reach out to your legislators and for extra credit the legislators serving on the relevant committees to ask them to support these policy priorities to improve maternal health in Iowa. Feel free to reach out to me at rachel.m.bruns @ gmail.com to discuss these policy priorities or other topics related to maternal health in Iowa.