Recently, the Health Policy Oversight Committee met and welcomed the new DHS Director, Kelly Garcia. Basically this committee provides oversight from the legislature for the Medicaid program.
Background
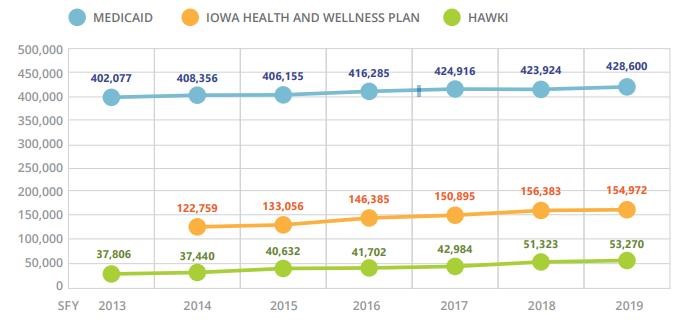
Medicaid in Iowa provides health insurance coverage for certain categories of low-income people (generally children, single parents with children, pregnant women, blind, disabled) under age 65 at or below 133% of the federal poverty level. Most Iowa Medicaid members are enrolled in Medicaid’s managed care program. These members will get health coverage from a Managed Care Organization (MCO). They get to choose between the 2 MCO’s that have contracted with Iowa: Amerigroup or Iowa Total Care. Total current Medicaid enrollment (blue line) is 428,600.
Iowa took the Medicaid expansion under Obama care in 2013. The expansion population took in all adults under age 65 at or below 133% of the federal poverty level. The expansion population is under what’s called the Iowa Health and Wellness Plan, which is basically the same health care coverage as Medicaid and the same managed care arrangement. Total current Iowa Health and Wellness Plan (Medicaid expansion) enrollment (orange line) is 154,972.
Last, there is the HAWK-I program, which is the children’s health
insurance program for those whose families’ incomes are too high to qualify for Medicaid but low enough that the children still are uninsured. Due to the families’ higher incomes, health care services through HAWK-I are less than those through Medicaid. These children are covered using the same MCO arrangement. Total current HAWK-I enrollment (green line) is 53,270.
Total current Iowa enrollment in state covered health care insurance (often all lumped together and called “Medicaid”) is 636,842. This is 20% of Iowa’s population, or 1 out of 5 Iowans.
This is a staggering number and makes Medicaid the fastest growing part of the Iowa budget. The state works to make sure all these people have access to services while at the same time ensuring schools, public safety, and other priorities are funded while keeping taxes as low as possible for Iowa’s citizens and to keep Iowa’s economic climate competitive and attractive for newcomers and businesses. This is why it is important for the state to periodically check and make sure that those who are on the program actually qualify. We want the resources not wasted on those who don’t qualify, but used for those who do qualify and are therefore the most in need.
Meeting Update
The committee first heard from the Iowa Medicaid Enterprise (IME) on the current Medicaid enrollment numbers and looked at how enrollment has trended since 2013. As you can see from the above chart, enrollment has been mostly trending slowly and steadily upward, with a few downturns here and there.
As for enrollment in the 2 MCO’s, there are currently 58.85% of members with Amerigroup and 41.15% with Iowa Total Care.
The committee then heard a presentation from IME on initial Medicaid eligibility and how members are verified to remain eligible for Medicaid as time goes on. IME utilizes multiple state and federal data sources to verify applicants/members income and eligibility, and requests specific information from the applicant/member if there is a question about either financial or non-financial eligibility requirements.
Member eligibility is then checked every 12 months and anytime there is a change it is reported to IME. Medicaid members are required to report any change in circumstances to IME within 10 days of the change. These changes include income, resources, household size, health insurance premiums or other health insurance coverage, and address. If a member fails to report a required change, the individual is then required to repay the state for any overpayment that occurred due to them not being eligible anymore.
Additionally, between application and annual review, there are multiple external income verifications that occur. Current computer data matching is exchanged between IME and the Social Security Administration, Iowa Workforce Development (wages and unemployment), Iowa Department of Public Health (death information), Public Assistance Reporting Information System (PARIS-receipt of benefits in multiple states), and Iowa Department of Corrections and county jails (incarceration). Before benefits are canceled for a member, the member is given a notice at least 10 days prior so they can provide additional information.
The Committee also heard an update on implementation of many legislated provider rate increases (EMS, disability providers, mental health treatment through Assertive Community Treatment Teams, rural hospitals and nursing homes) and process changes to benefit Medicaid members.
IME Director Randol announced that since July, IME has been able to add 71 kids to receive services under the Children’s Mental Health Waiver, after opening 400 slots from additional state funding.
Director Randol also announced that a uniform prior authorization form has been created for inpatient services and outpatient services, and that the MCOs are currently reviewing those draft forms. The goal is to have these universal forms available to providers by early 2020.
Lastly, IME meets twice weekly with each MCO to resolve specific claims issues and has maintained a claim reserve with UnitedHealthCare, the MCO which has recently left the state. IME monitors all provider claims on a monthly basis to ensure that United has paid providers before completely exiting the Iowa program. Please reach out to me if you are a Medicaid member or provider that needs assistance navigating the system or working with your MCO.